The UK public sector is in a productivity crisis. As Chancellor Jeremy Hunt has set out, since the pandemic, the private sector has seen a 1.3% uplift in productivity, but public services are still 5.7% less productive than they were before Covid hit.
The intent in the National Health Service is to return activity and productivity to pre-pandemic levels, However, data shows that in 2022/23 the NHS offered 400,000 fewer outpatient appointments compared to in 2019/20 and a recent analysis conducted by the Health Foundation think-tank found that if hospital elective care activity remains the same, and strikes stop, waiting lists for NHS elective care services could rise to 8 million by summer 2024.
The NHS productivity puzzle
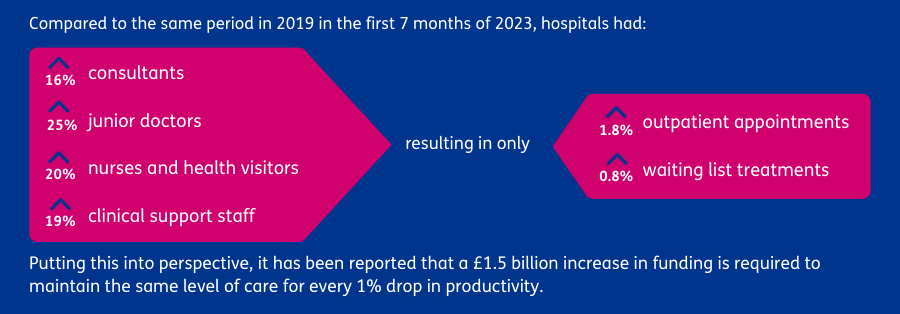
We know from speaking with our NHS clients that the productivity puzzle is real: whilst there has been an increase in funding, and in workforce size, hospital activity and productivity has not increased proportionately.
This does not mean however that all health and social care sectors have experienced the same trend. A record 25 million potentially lifesaving checks and tests took place last year, 2 million more than compared to the same period before the pandemic. In Primary Care, 4 million more GP patient appointments a month are being delivered compared to before the pandemic, with comparatively fewer fully qualified GPs in post.
However, despite some of these counterfactuals, our Health Team at Baringa believe that productivity in the NHS is a national challenge that needs to be addressed. Life expectancy is increasing, citizens have more complex health needs, demand will continue to rise, and funding for NHS services is likely to remain static for much of the remaining decade. The need to deliver ‘more for less’ has never been greater.
What is driving the productivity challenge?
Whilst the acute sector is often at the centre of productivity discussions, we know from our conversations with senior NHS leaders that these trends, and the corresponding opportunities, exist across the whole system.
We highlight trends across four key themes that are directly contributing to the productivity challenge:
- Morale and motivation – The 2022 NHS staff survey shows a decline in the measure for staff morale and how staff feel about recognition and rewards, both key drivers of productivity. Other causes for concern include the willingness of staff to recommend the NHS as a place to work’, falling from 59.4% to 57.4%. The ongoing strike actions will have further impacted low morale and motivation.
- Resource and capability gaps – Consistently high sickness and attrition rates across the NHS persist, with NHS staff sickness rates 29% higher in 2022 compared to 2019. This not only leads to reduced capacity, and heightened reliance on temporary staffing to treat patients, but also the loss of tacit knowledge and experience. Many leaders have also sighted a significant loss of core management capability to drive performance.
- Bureaucracy and competing priorities – There is a spotlight on identifying opportunities to improve productivity, but the ability of NHS leaders to drive innovation and achieve long-term goals can often be constrained by competing national priorities, bureaucracy and regulations, and a constant pressure to meet national targets.
- Capital investment – Capital investment is required to fund the renovation and construction of hospitals and other care settings, to invest in better medical technology, and enhance digital capabilities, all of which aid productivity. Yet historically capital funding has been used to address short-term revenue deficits rather than being ring-fenced to support longer-term priorities. What limited capital funding is then available tends to be reactively allocated and invariably distributed across systems.
How can we tackle the productivity challenge?
Baringa believes that there are a number of areas that will have a fundamental impact on tackling productivity:
- A shift to purpose-led performance - At Baringa, we believe that an important step is to shift mindsets from focusing on traditional productivity measures, such as levels of activity, to those that are purpose-led and outcome-focused. Baringa’s “Purpose Led Performance” framework puts purpose at the core, focused on empowering organisations to define and measure the value of their work in relation to what matters most. Levers such as defining and measuring outcomes against core purpose, using data to drive effective decision making, and improving communication and collaboration to scale success are central to this framework. The NHS needs to be more ambitious and move towards this change in approach to align targets and accountability. Leeds Teaching Hospitals and the Yorkshire Ambulance Service are a good example of this. These trusts worked together to develop solutions and a shared purpose for their work on maintaining a lower number of ambulance handover delays. This joined up working allowed everyone to take a shared responsibility for finding the right solution to radically reduce ambulance hand over times; in January 2023, their sites achieved over 99% of handovers within 1 hour, no doubt improving patient outcomes and experience.
- Leveraging the use of data and technology - The NHS is not short of data; however available data needs to be used in a more sophisticated way to account for quality and overall care outcomes when measuring productivity. This cannot be achieved without access to accurate data that is available in real-time. Whilst the scaling of self-service analytics in the healthcare sector is a top priority for the NHSE priority, further work is required to embed a culture of data-led decision making a better picture of productivity. Technology is also cited as one of the biggest enablers to boosting productivity and this is no different in healthcare where artificial intelligence (AI) is already being leveraged to find efficiencies in both operational and clinical workflows. Embracing a digital mindset and culture, and emerging technology such as AI, will be fundamental in realising technology and data-driven productivity gains.
- System wide collaboration - One of the core purposes of ICSs is to ‘enhance productivity and value for money’ by working collaboratively to scale innovation and make better use of resources to drive economies of scale. There are good examples of where this has been applied to increase productivity: for example, the Mental Health, Learning Disabilities and Autism (MHLDA) provider collaboratives worked together to deliver a pilot across 15 sites that resulted in a 70% reduction in admissions and over £30m in savings. However, more needs to be done to shift to this new way of working and government powers need to ensure that system organisations have the agility to work together to drive transformation at pace.
Baringa has experience of tackling productivity challenges across various sectors. We want to bring our broader industry insights, coupled with our deep health sector knowledge, to engage NHS leaders in innovative discussions to tackle the productivity challenge together. We will be holding a series of roundtable discussions in April with NHS leaders to debate the productivity puzzle and the solutions that can be scaled up across local and national geographies.
If you would like to register for these events subscribe here.
Our Experts


Related Insights

From engagement to improvement: how empowering civil servants leads to better outcomes
Taking a people-led change approach, focusing first on fostering a positive team culture and boosting employee morale, drives significant improvements.
Read more
How to create inspiring leaders in government
Discover the three key ways Baringa’s leadership programme is critical to tackling backlogs, increasing case management throughput, and boosting employee satisfaction.
Read more
People power: how government can be more productive by empowering its people
Baringa’s Team-by-Team (TbT) approach helps Government departments and agencies to become more productive by focusing on their people and making sure they feel empowered to deliver on key outcomes.
Read more
Departments must not obsess over ‘input measures’ when developing productivity plans – especially when it comes to tracking time
Government organisations need to be mindful of the cost they are creating around input measures.
Read moreRelated Case Studies

Building the UK’s critical Covid-19 Test & Trace infrastructure
How do we drive procurement success during the biggest global health crisis of the last century?
Read more
Bringing best practice to a major government department
We created measurable programme progress and raised the departments' credibility to deliver with ministers.
Read more
Shaping a government department’s net zero portfolio delivery approach
Achieving net zero emissions is one of the most pivotal and complex economy-wide transformations in UK government history. How do we measure progress and prioritise initiatives to make the biggest impact?
Read more
We designed the NHS Covid vaccine supply chain, putting patients at its centre
With Covid numbers rising, and first vaccines coming to market, the NHS needed an agile and resilient vaccine supply chain to deliver millions of jabs to the country.
Read more